Hong Kong West Cluster
Table HKW-1. Antibiogram for all isolates, HKW, 2021
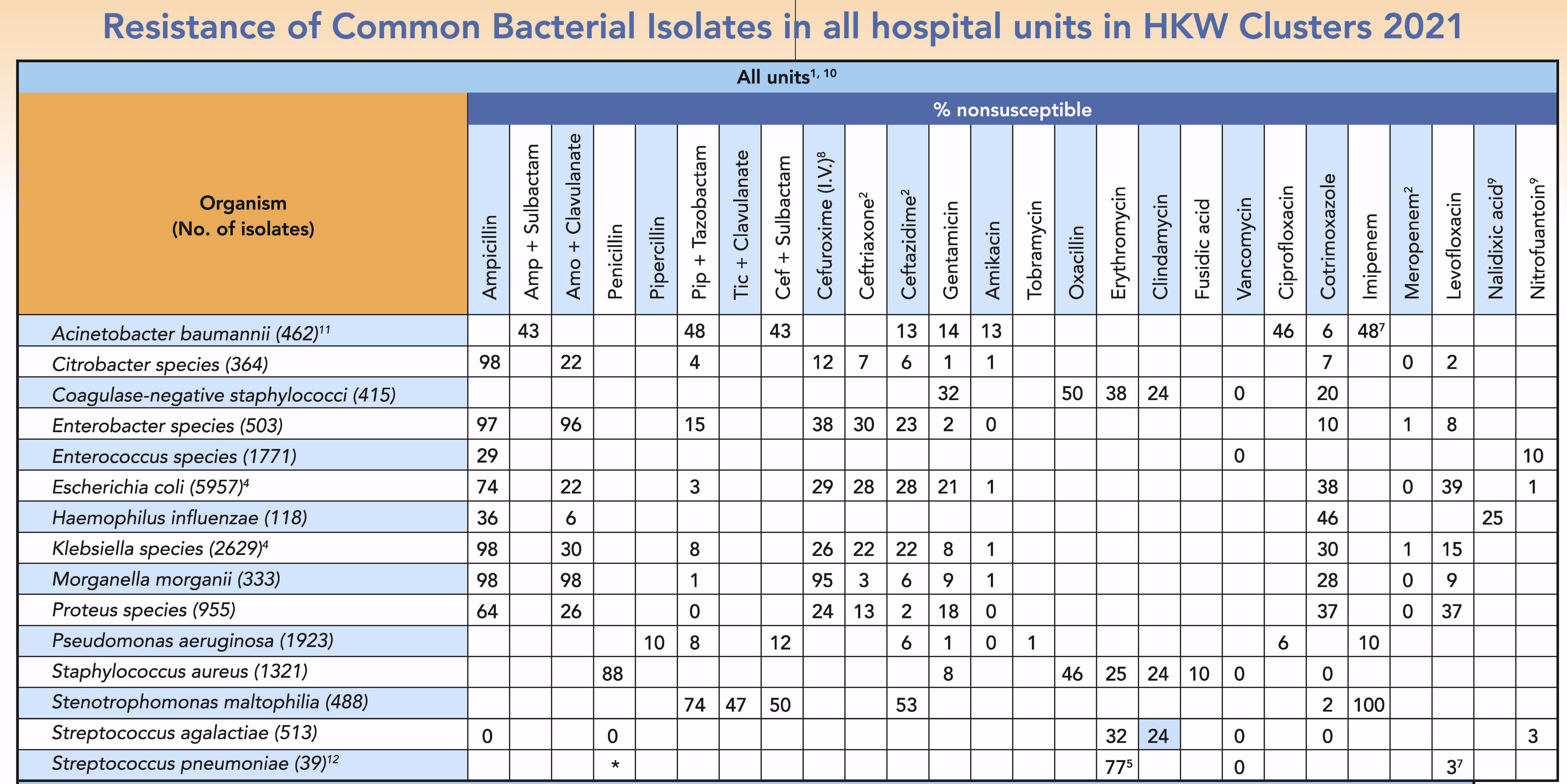
- Non-duplicate isolates from blood, urine and respiratory specimens. Interpreted according to CLSI M100-S28 2021. Nonsusceptible includes both intermediate and resistant.
- Results for Enterobacteriaceae were interpreted according to CLSI M100-S28 2021. A total of 40 sporadic carbapenemase-producing Enterobacteriaceae (CPE) isolates were detected in 36 patients. The specimen sources include blood (n=9), respiratory (n=5), and urine (n=26). The 40 isolates produced NDM (n=26), OXA-48 (n=7), and KPC (n=7) types of carbapenemases.
- Ho PL Int J Antimicrob Agents 2010;36:469 and J Hosp Infect 2010;74:358
- Overall prevalence of extended-spectrum beta-lactamases (ESBL) was 22% for Klebsiella species and 28% for E. coli. ESBL-producing strains should be interpreted as resistant to all penicillins, cephalosporins, and aztreonam.
- In S. pneumoniae, resistance to azithromycin & clarithromycin can be predicted by testing erythromycin (CLSI M100-S28 2021).
- Most had other risk factors such as past hospitalization and nursing home residence.
- Ho PL J Antimicrob Chemo 2009;63:836
- According to breakpoint for parenteral cefuroxime sodium.
- Urine isolates only.
-
, indicate 10% or more reduction in resistance rate compared to 2020.
, indicate ≥10% increase in resistance rate compared to 2020. - The figure refers to ACB complex, including Acinetobacter baumannii, Acinetobacter calcoaceticus, Acinetobacter nosocomialis, and Acinetobacter pittii.
- Combined data from 2020(17) and 2021(22)
* Including MIC ≤ 0.06 (30.8%), MIC 0.09-1 (46.2%), MIC 1.5-2 (15.4%), MIC 3-6 (5.1%), MIC 8 (2.6%)
% Penicillin sensitive: meningitis breakpoint at MIC ≤0.06 = 30.8% and non-meningitis breakpoint at MIC≤2 = 92.3%
Abbreviation: Amp, Ampicillin; Amo, Amoxicillin; Pip, Piperacillin; Tic, Ticarcillin; Cef, Cefoperazone