Part VII: Other Issues
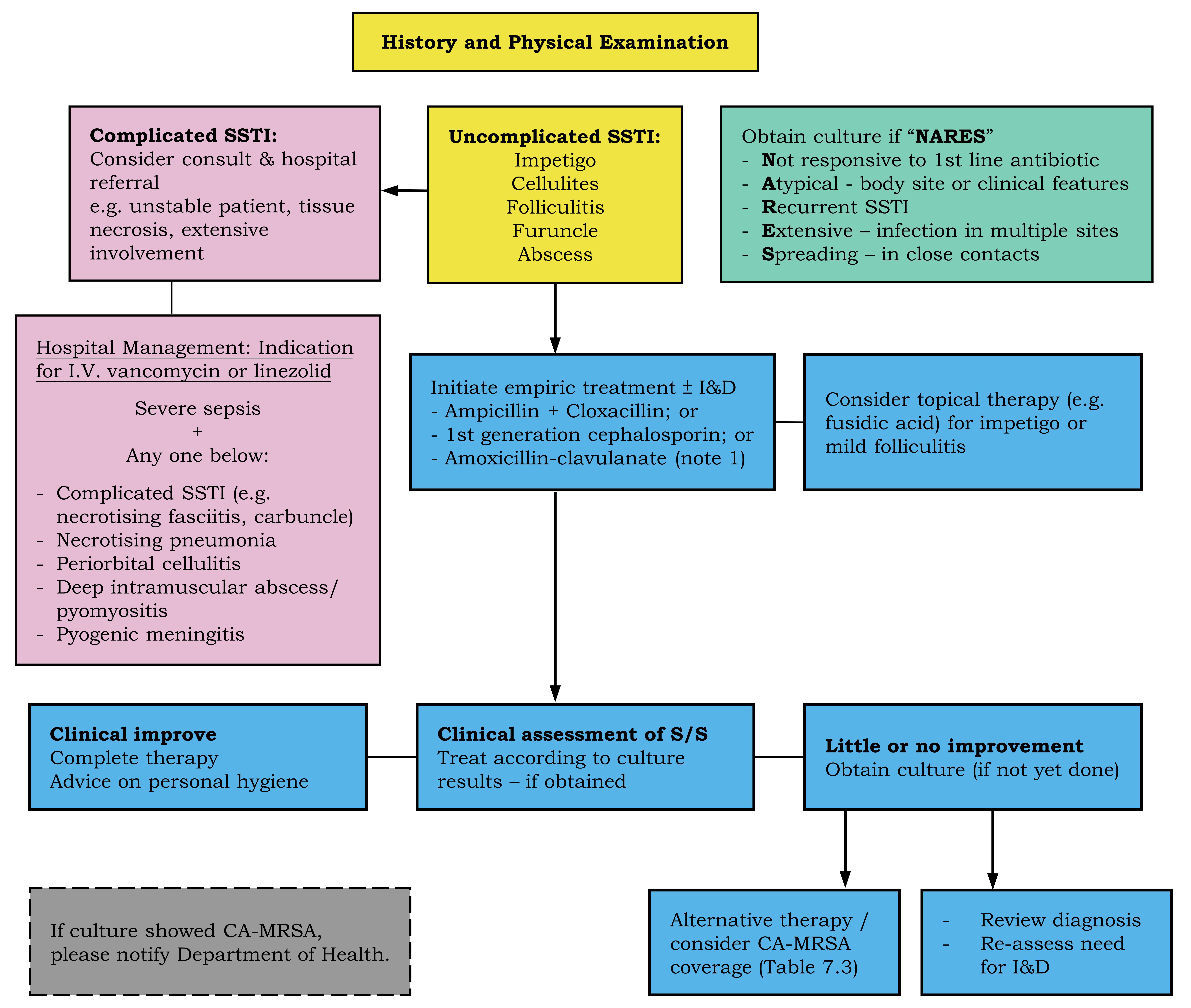
7.2 Clinical Guideline for Management of Suspected/Confirmed CA-MRSA Infections
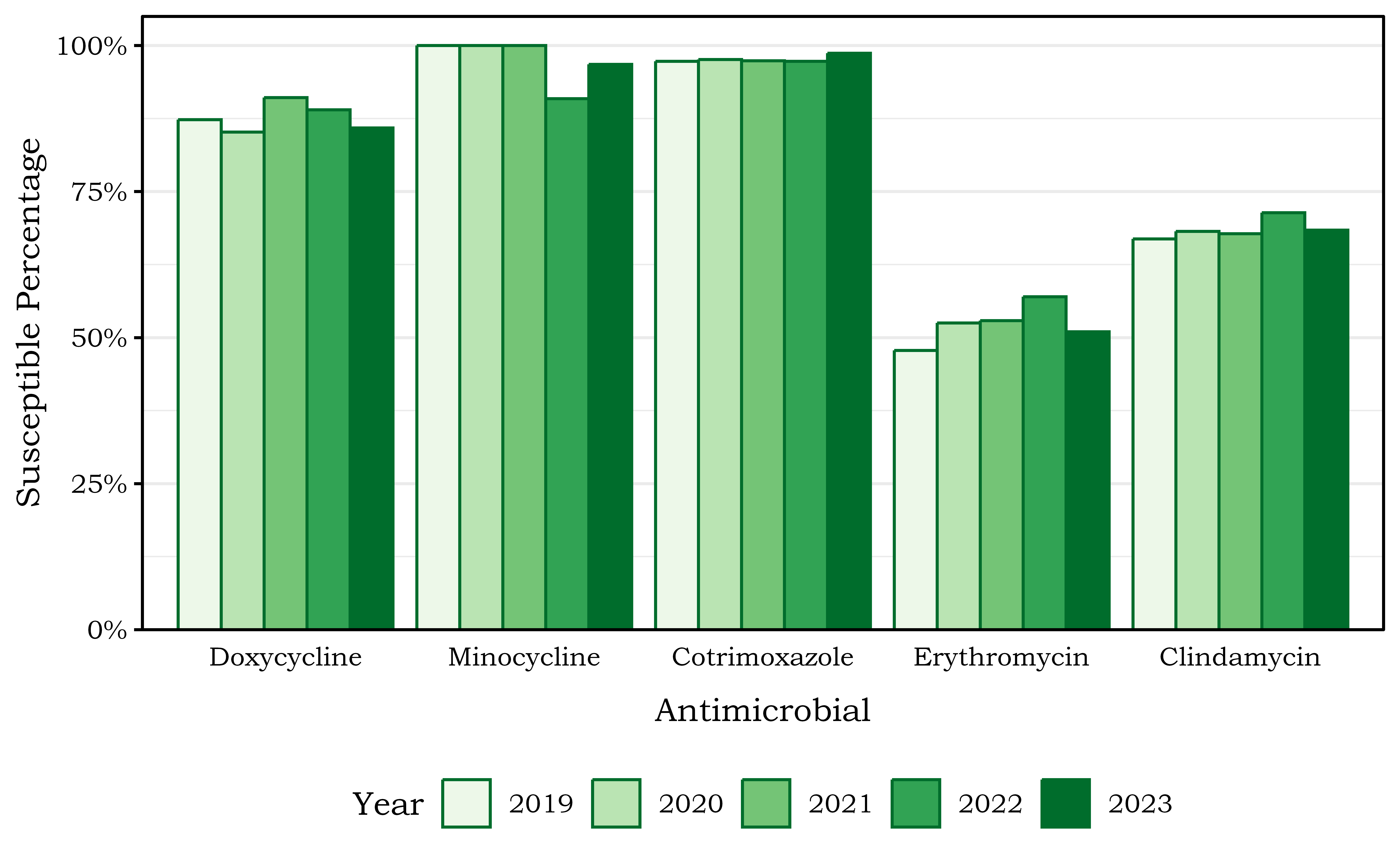
AgentFootnote 1–3 |
Potential advantage |
Precautions |
Usual dose for adult |
|---|---|---|---|
Cotrimoxazole (Septrin) |
Oral |
Not for patients with sulphur allergy |
P.O. 960 mg b.i.d. |
Doxycycline/ minocycline |
High skin concentration |
Not for children <8y or pregnant women [526] |
P.O. 200 mg once, then 100 mg b.i.d. |
Clindamycin |
Inhibit toxin production |
Footnote 4 |
P.O. 300–450 mg tds |
|
Footnotes: 1. Clinicians should consult complete drug prescribing information. Antibiotic therapy should be modified according to results of culture and susceptibility testing. Information available at present showed that most CA-MRSA isolates in HKSAR are susceptible to the above oral antibiotics. The duration of therapy for most SSTI is 5 to 7 days; longer therapy (10 days) is necessary for more severe infection (e.g. if patient is febrile &/or abscess size >5cm). 2. Oral antibiotics are not indicated for MRSA carriage/colonisation. 3. Abscess with size <5cm may resolve with incision & drainage alone. Treatment with antibiotic might have higher cure rate and is important if patient is febrile &/or abscess size >5cm. [176,527,528] 4. If clindamycin is considered, isolate resistant to erythromycin but with apparent “sensitivity” to clindamycin should undergo laboratory testing for inducible clindamycin resistance using the ‘D’ test (flattening of the clindamycin zone adjacent to the erythromycin disc). |
|||