Part I: Antibiotic Resistance (AMR) - Global and Local Epidemiology
1.5 Extended-spectrum β-lactamase producing Enterobacterales (ESBL-E)
-
ESBLs are enzymes capable of hydrolysing penicillin, first-, second- and third-generation (extended-spectrum) cephalosporins and aztreonam (except the cephamycins and carbapenems). Most ESBLs can be inhibited by β-lactamase inhibitors such as clavulanate and tazobactam (Table 1.6). [46] TEM, SHV and CTX-M are the three most common families of ESBLs seen worldwide.
-
In Hong Kong (Figure 1.3), >90% of strains with an ESBL phenotype produced CTX-M type enzymes. [47,48] There is a high rate of resistance towards non-β-lactam antibiotics, particularly fluoroquinolones, cotrimoxazole and aminoglycosides. [47,48] The high rate of resistance to non-β-lactam antibiotics therefore limits the choice for management of patients in outpatient setting.
ESBL-E has been considered to be a hospital pathogen in the past. However, community-onset infection has been described in different countries including Hong Kong in recent years. Most of the patients presented with lower urinary tract infection, other presentations include bacteraemia and intra-abdominal infection. [49–52]
-
In a local population-based study in 2017, ESBL-E was detected in 52.8% of stool samples in healthy individuals. [53] Food animals are a major reservoir of ESBL-producing E. coli. [54,55] Local surveillance data by the Centre for Health Protection revealed presence of ESBL-E in 77.8% of beef, 80.7% of pork and 99.7% of chicken. [56] It is also worth noting that ESBL-E is also commonly found in ready-to-eat (RTE) foods such as siu mei, lo mei, sashimi, sushi, RTE vegetables and cut fruits. [57]
-
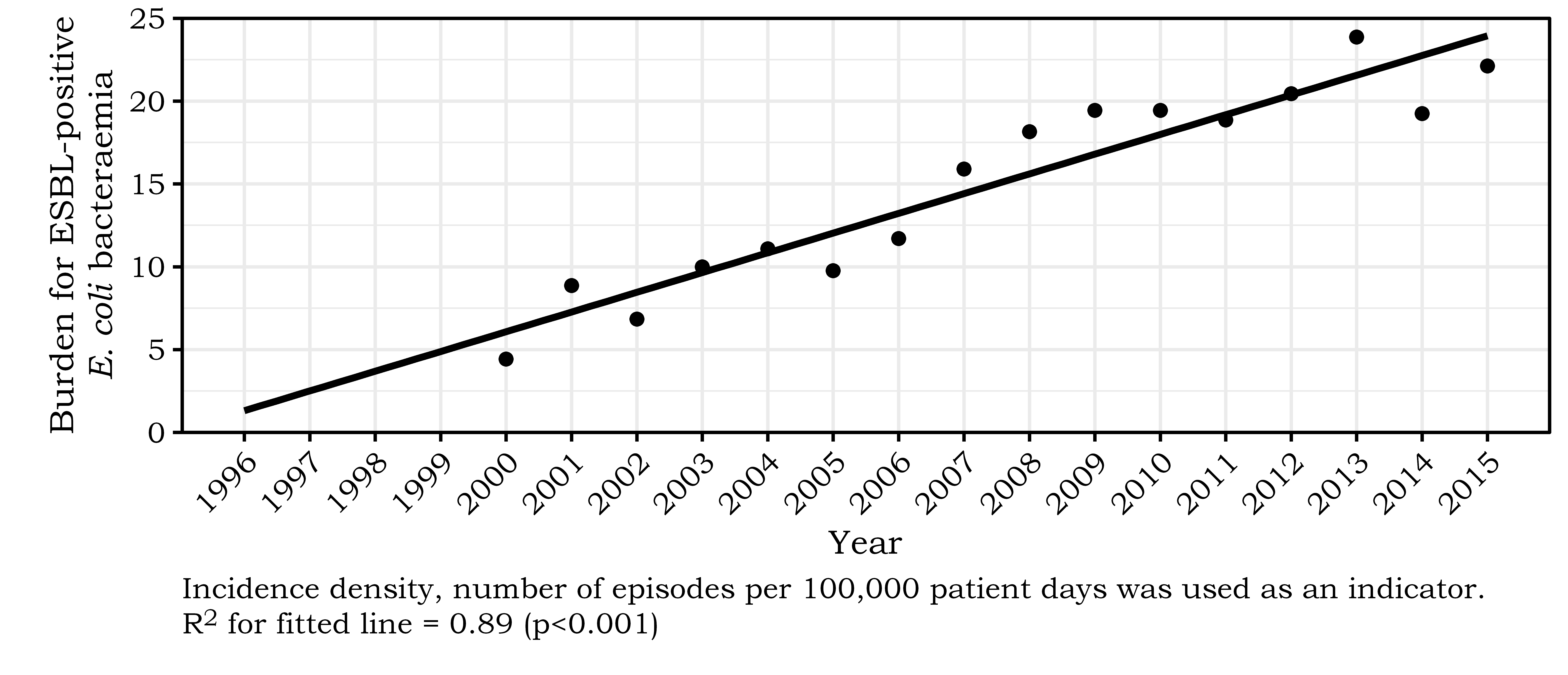
In Hong Kong, the burden of ESBL-E is highest among the elderly population, especially those aged 75 years and above. [58]
-
For two decades, ESBL-E were considered to be clinically resistant to all cephalosporins. Accordingly, all laboratories are advised to edit the results for ceftazidime, ceftriaxone and cefepime to resistant, irrespective of the in vitro inhibition zone diameters or MIC values. [59]
-
Recently, the laboratory testing advisory bodies in the United States and Europe have revised their advice and argued that with the lowered cephalosporin breakpoints that both organisations now adopted, it is unnecessary to edit susceptibility categories if an ESBL is found. [60,61] A group of international experts in this field considered such advice is misguided. [59] Therefore, it is prudent to continue to test for the presence of ESBLs directly and to avoid cephalosporins as treatment.
-
In Hong Kong, if we apply the new ceftazidime breakpoint, three-quarters of the ESBL-producing isolates would be re-classified from resistant to susceptible to ceftazidime. [62] Caution with this approach is necessary whilst clinical data are limited. [59]
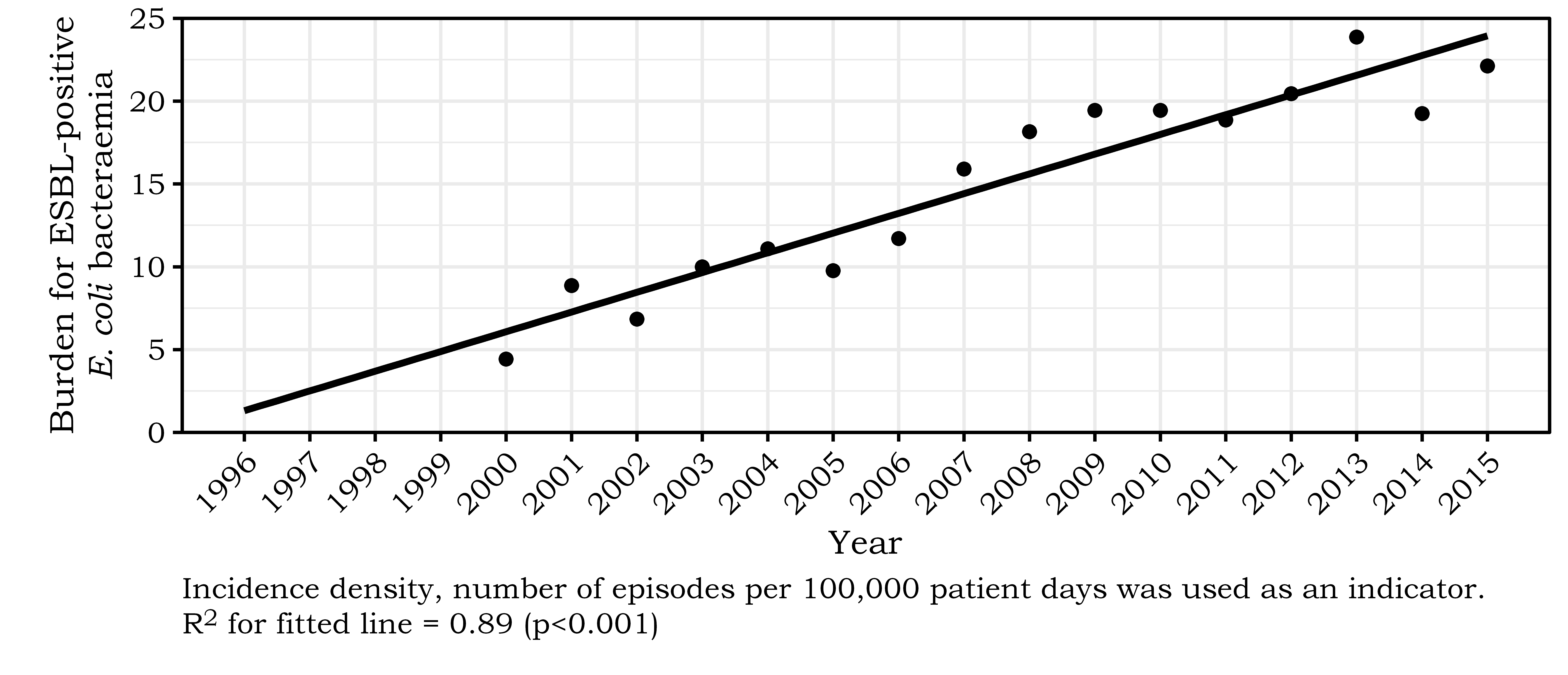
Reference: [58]
|
ESBL |
AmpC β-lactamase |
|---|---|---|
Bush-Jacoby-Medeiros functional class |
2be |
|
Ambler molecular classification |
A |
C |
Plasmid mediated |
Almost always (responsible for the spread) |
Most are chromosomal |
Inhibition by clavulanate, tazobactam, sulbactam* |
Inhibited |
Not inhibited |
Cephamycins |
Not hydrolysed |
Hydrolysed |
Oxyimino-β-lactams |
Hydrolysed |
Hydrolysed |
Cefepime |
Variable |
Not hydrolysed |
Carbapenem |
Not hydrolysed |
Not hydrolysed |
Examples |
TEM, SHV and CTX-M |
Enterobacter, Citrobacter and Serratia possess inducible AmpC β-lactamase encoded in their chromosomes |
*β-lactamase inhibitor |
||