Part I: Antibiotic Resistance (AMR) - Global and Local Epidemiology
1.3 Methicillin-resistant Staphylococcus aureus (MRSA)
MRSA are resistant to penicillins (including cloxacillin and flucloxacillin), β-lactam/β-lactamase inhibitor combinations, cephalosporins, and carbapenems due to alterations in penicillin binding protein. Only the new anti-MRSA β-lactams (e.g. ceftaroline) remain effective against MRSA. However, reduced susceptibility to ceftaroline has recently been reported both in vitro and in vivo. [16,17]
MRSA is classified into healthcare-associated (HA-MRSA) and community-associated (CA-MRSA). The United States Centers for Disease Control and Prevention (CDC) classification, which is the most widely accepted, classified HA-MRSA and CA-MRSA epidemiologically. [18] However, the border between the two is becoming blurred and surveillance using epidemiological criteria alone has become insufficient.
HA-MRSA
-
Vancomycin is less effective than anti-staphylococcal β-lactams for methicillin-susceptible S. aureus (MSSA) infections. [19] However, vancomycin remains the treatment of choice for infections caused by MRSA. The efficacy of vancomycin may be compromised by factors such as the lower potency of generic formulations, suboptimal dosing, limited tissue penetration, slow bactericidal activity, and strains of MRSA with reduced susceptibility to the drug. [19–21]
The susceptibility profile is not a distinguishing factor between HA-MRSA and CA-MRSA. Local hospitals have seen a rise in multi-susceptible MRSA prevalence in recent years. These MRSA are classified as HA-MRSA and are linked to the spread of the ST45/t1081 clone carrying SCCmec type IV or V. About 75% of these isolates were identified in residents of elderly care facilities, suggesting a potential for increased transmission among this population, serving as a reservoir. [22]
In 2011, a local study on MRSA carriage at admission to 15 acute medical units showed that the overall carriage rate was 14.3%. [23] Risk factors include MRSA history within the past 12 months, old age home residence, and bed-bound state. Molecular typing revealed that ST45/t1081 is a major clone circulating among the patients. [23]
A study conducted locally between 2015 and 2018 revealed that 2.1% of patients were carriers of gastrointestinal MRSA upon admission screening, with ST45 being the predominant sequence type. [24]
-
A 2021 local study discovered that 48.7% of elderly home residents carried MRSA at any body site, while 8.5% of staff members were nasal MRSA carriers, predominantly of the ST1047 lineage 1. [25]
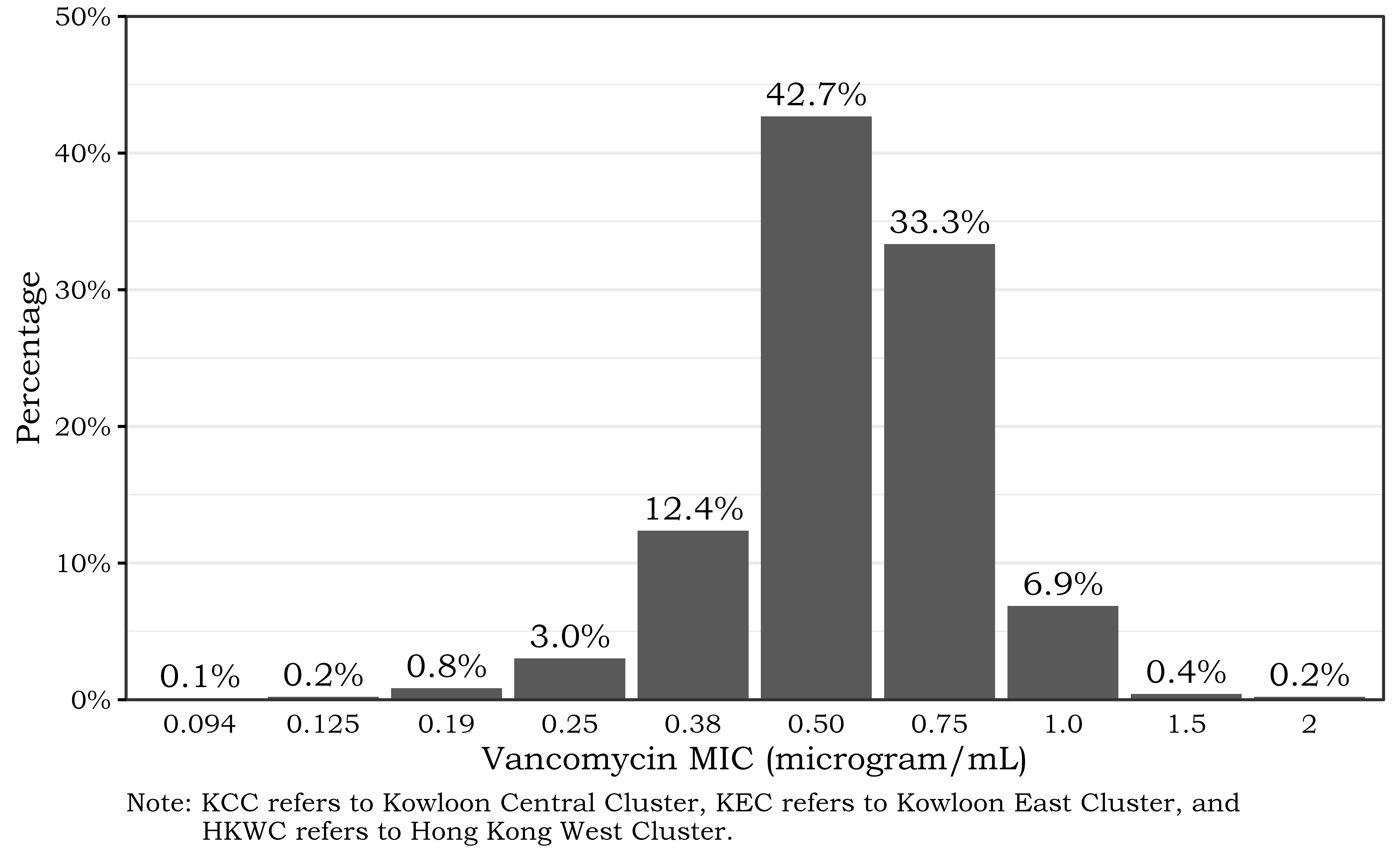
- The vancomycin MIC of 3 public hospitals between 2020–2023 showed that majority of the isolates had MIC ≤1 microgram/mL.
CA-MRSA
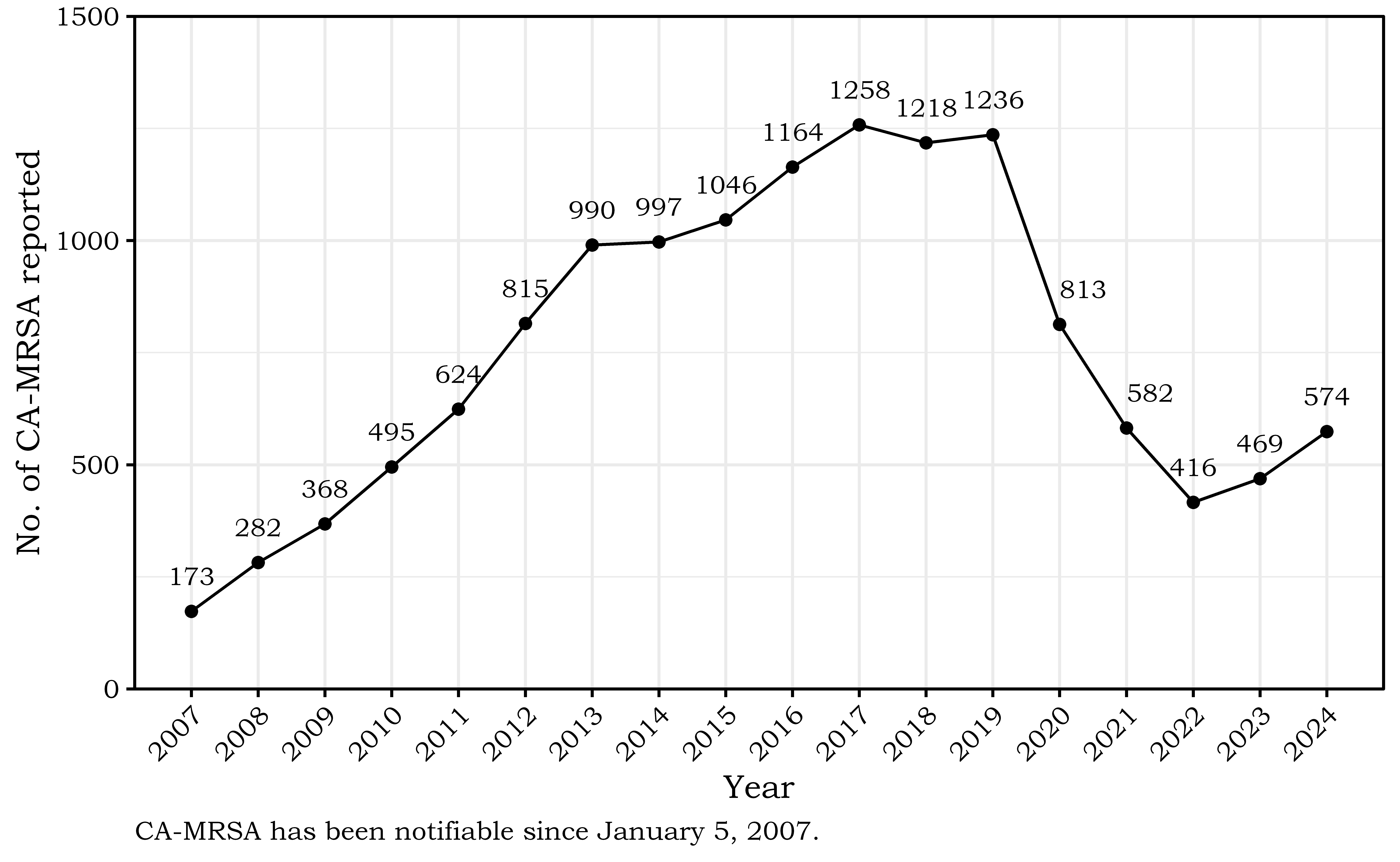
CA-MRSA was initially documented in Hong Kong in 2001 and has shown rapid emergence over the past two decades. It has been designated as a notifiable disease, necessitating reporting to the Department of Health (DH) since January 2007 (Figure 1.2). The number of cases has steadily risen to over 1,000 per year, with a subsequent decrease during the COVID-19 pandemic. [26]
It is responsible for 10.4% of purulent cellulitis and 5% of cutaneous abscess in the Accident & Emergency setting. [27]
During the period from January 2012 to October 2015, 3,650 cases of CA-MRSA were documented, of which 98% were uncomplicated skin and soft tissue infections, and 2% were invasive CA-MRSA infections, resulting in four fatalities. [28]
Patients infected with CA-MRSA do not have the usual risk factors associated with HA-MRSA. Locally, case control studies revealed that ethnic minority and sharing of personal items with other persons were risk factors for CA-MRSA while frequent hand washing was protective against CA-MRSA infection. [29,30]
-
Panton-Valentine leukocidin (PVL) toxin is a pore forming cytotoxin that is capable of destroying human monocytes and neutrophils. PVL toxin has been associated with virulence and transmissibility of CA-MRSA. While presence of PVL toxin in MRSA is used as a criterion for reporting of CA-MRSA in Hong Kong, it has been shown that some of the CA-MRSA causing skin and soft tissue infection were PVL negative. [29]
Other than skin and soft tissue infections, PVL toxin is also associated with necrotising pneumonia, necrotising fasciitis and meningitis. CA-MRSA has also been reported to co-infect with influenza resulting in fulminant pneumonia. [31–33]