Private Hospitals
Table GHK. Antibiogram for common bacterial isolates, Gleneagles Hospital Hong Kong, 2024
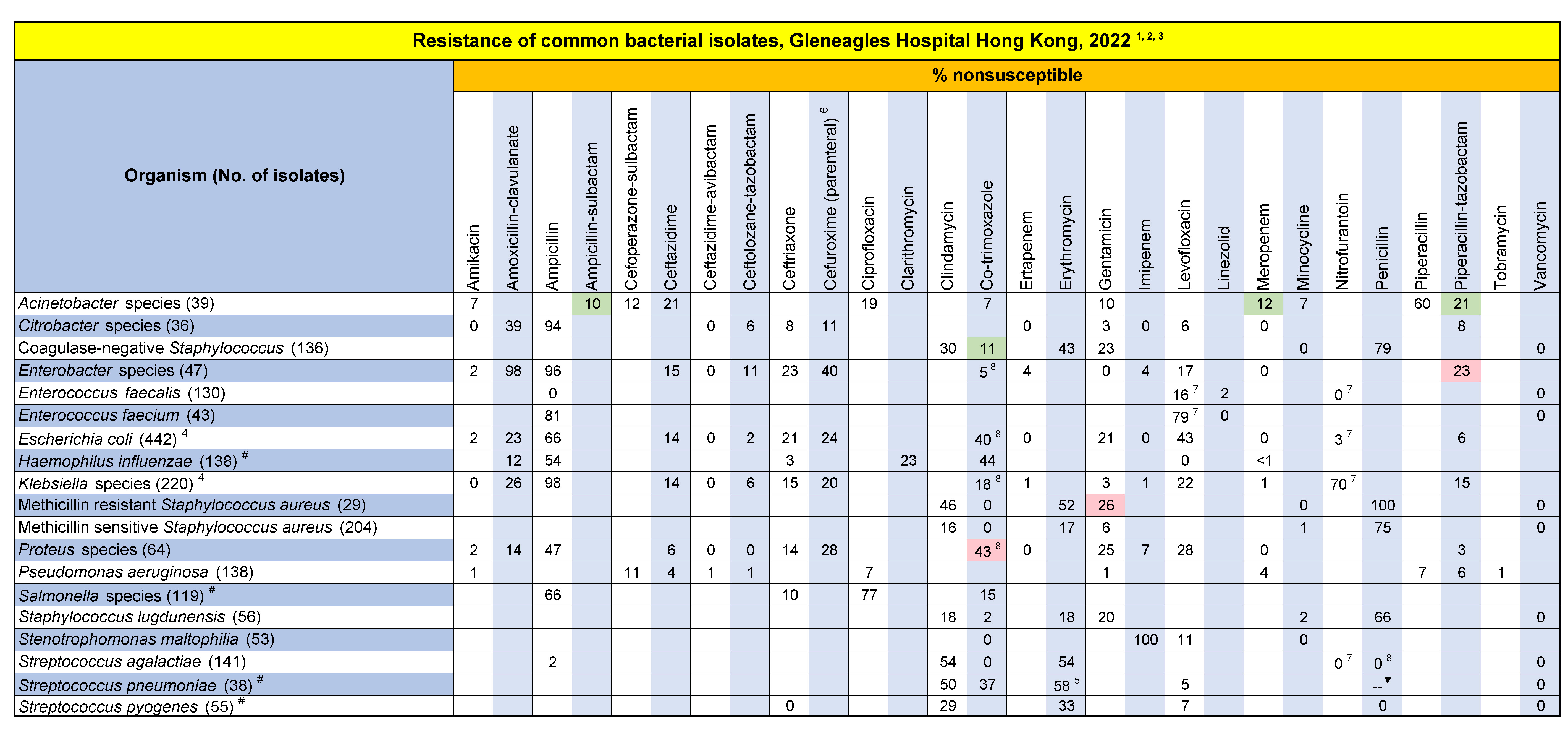
- Only the first isolates of a given species per patient per calendar year were included, irrespective of body site, antimicrobial susceptibility profile or other phenotypical characteristics.
Susceptibility results were only given when not less than 30 isolates were collected. - Results obtained from surveillance studies (MRSA Screening, CPE Screening, VRE Screening and GBS Screening) were excluded.
- Susceptibility results were interpreted according to 2024 CLSI definition except Cefoperazone-sulbactam (Sulperazon) which was with reference to Pfizer 2019. Nonsusceptible included both intermediate and resistant.
- Overall prevalance of extended-spectrum beta-lactamases (ESBL) were 14.1% for Klebsiella species, 22.5% for E. coli. ESBL-producing strains should be interpreted as resistant to all penicillins, cephalosporins and aztreonam.
- In Streptococcus pneumoniae, resistance to azithromycin & clarithromycin can be predicted by testing erythromycin (CLSI M100).
- According to breakpoint for parenteral cefuroxime sodium.
- Results obtained from urine isolates only.
- Results obtained from non urine isolates only.
For Streptococcus pneumoniae, Penicillin (parenteral) MIC ≤0.06 µg/mL (75.9%), MIC 0.09-1 µg/mL (6.9%), MIC 1.5-2 µg/mL (10.3%), MIC 4 µg/mL (6.9%).
% Penicillin (parenteral) sensitive: non-meningitis breakpoint at MIC ≤2 µg/mL = 93.1% and meningitis breakpoint at MIC ≤0.06 µg/mL = 75.9%.
# The annual number of isolates is small. Data from 2023 to 2024 were combined in the calculation.
Indicate 10% or more reduction in annual resistant rate compared to 2023 figures.