Home > Chapters
Chapters
Part II: Antimicrobial stewardship programme
2.2 Tips on safe use of antibiotics in outpatient setting
- Understand the local prevalence of pathogens and associated antibiotic susceptibility profiles. Information on surveillance of AMR at community outpatient setting is available at the CHP webpage (128).
- Management of patients with respiratory tract infections should be personalised. A careful clinical evaluation (e.g. patient’s age, underlying comorbidity, duration and severity of symptoms, physical findings) is essential in making decision to use or to avoid antibiotics. Upper respiratory tract infections are often viral in origin. In a study, antibiotics were prescribed in 68% of visits for symptoms of acute respiratory tract infections; among those, 80% were unnecessary according to CDC guidelines (129). Clinical discrimination is required in using clinic-based, point-of-care testing (e.g. flu A and B, C-reactive protein, white blood cell (WBC), urinalysis).
- It is a good clinical practice to explain to the patient the reasons for giving or not giving antibiotics (130) and to provide information on the average total length of the illness (131) as below:
- Acute otitis media: 4 days
- Acute sore throat/acute pharyngitis/acute tonsillitis: 1 week
- Common cold: up to 10 days
- Acute rhinosinusitis: 2 to 3 weeks
- Acute bronchitis: 3 weeks
- Whenever appropriate, prescribe the simplest regimen and shortest duration of treatment (132).
- Take an ‘antibiotic timeout’ if possible, e.g. reassessing need of antibiotics after 48–72 hours.
- Advise patients to observe the following precautions while on antibiotics (Figure 2.1):
- Practice frequent hand hygiene;
- Eat or drink only thoroughly cooked or boiled items;
- Disinfect and cover all wounds;
- Wear mask if he/she has respiratory symptoms;
- Young children with symptoms of infection should minimise contact with other children.
- Take the opportunity to educate patients on proper use of antibiotics:
- Only take antibiotics prescribed for him/her;
- Do not share or use leftover antibiotics;
- Do not save antibiotics for the next illness;
- Do not ask for antibiotics when your doctor thinks you do not need them. In a study of paediatric care, doctors prescribe antibiotics 62% of the time if they perceive pressure from parents and 7% of the time if they feel parents do not expect them (133).
Figure 2.1 Cue card for patient education
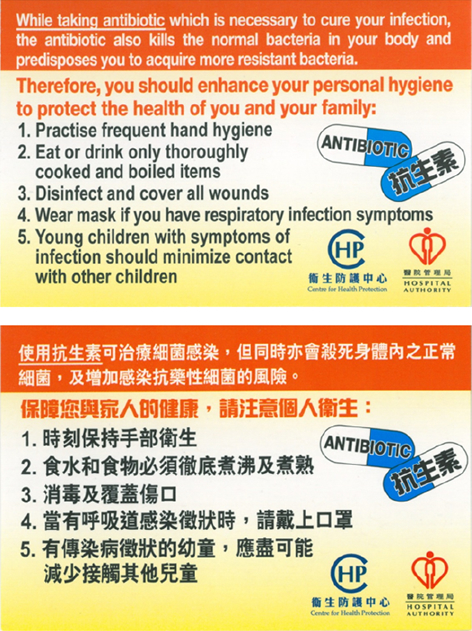
Table 2.2 Core elements of outpatient ASP (134)
| Commitment |
|
| Action for policy and practice |
|
| Tracking and reporting |
|
| Education and expertise |
|